
Kenya’s Preparedness for Future Pandemics: Lessons from COVID-19
Introduction
The COVID-19 pandemic was a wake-up call for the global community, revealing both strengths and vulnerabilities in health systems, economies, and governance. For Kenya, the pandemic highlighted the urgent need for preparedness against future health crises. While the country faced challenges in managing the immediate effects of COVID-19, it also gained valuable lessons that are now shaping its approach to pandemic preparedness. This blog explores Kenya’s response to COVID-19, the lessons learned, and the steps the country is taking to strengthen its preparedness for future pandemics.
Kenya’s Response to the COVID-19 Pandemic

1. Initial Challenges in Managing the Pandemic
Kenya’s response to the COVID-19 pandemic began in March 2020 when the first case was confirmed. The country faced immediate challenges in terms of healthcare infrastructure, medical supplies, and the capacity to handle large-scale public health emergencies. With a relatively underfunded healthcare system, Kenya struggled to provide adequate care to COVID-19 patients, especially during the early days of the pandemic.
Key challenges included:
- Inadequate healthcare infrastructure: Many hospitals lacked the necessary equipment, including ventilators and personal protective equipment (PPE).
- Overburdened healthcare workers: The pandemic put significant strain on healthcare workers, who were at risk of infection while handling COVID-19 cases.
- Supply chain disruptions: Kenya faced difficulties in obtaining essential medical supplies and vaccines due to global competition and logistical challenges.
Despite these obstacles, Kenya implemented various public health measures, such as lockdowns, curfews, and mask mandates, to curb the spread of the virus.
2. Government and Public Health Interventions

The Kenyan government quickly mobilized resources to combat the pandemic. The Ministry of Health, with support from international partners, launched several initiatives, including:
- Testing and contact tracing: Testing centers were set up across the country to detect COVID-19 cases. The government also implemented contact tracing measures to identify individuals who had been exposed to the virus.
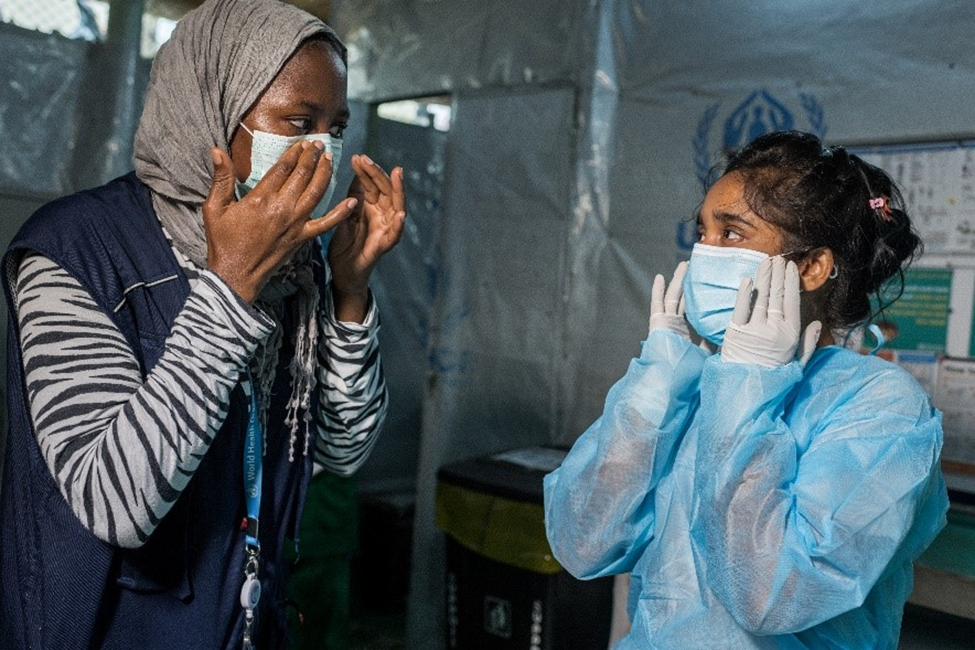
- Vaccination campaigns: Once vaccines became available, Kenya initiated mass vaccination campaigns, focusing on vulnerable populations such as healthcare workers, the elderly, and individuals with underlying conditions.
- Public awareness campaigns: The government launched information campaigns to educate the public on preventive measures, such as social distancing, handwashing, and mask-wearing.
Though these efforts were commendable, they revealed the need for a more robust and coordinated response to future pandemics.
Lessons Learned from the COVID-19 Pandemic
1. Strengthening Healthcare Infrastructure

One of the most significant lessons from the COVID-19 pandemic is the need to invest in healthcare infrastructure. The pandemic exposed weaknesses in Kenya’s healthcare system, especially in terms of the availability of medical equipment, the number of healthcare professionals, and the ability to provide critical care during a surge in cases.
- Investing in healthcare facilities: Expanding the capacity of hospitals and healthcare centers, particularly in rural and underserved areas, is critical. This includes building more isolation wards, increasing the number of intensive care unit (ICU) beds, and improving the supply of essential medical equipment.
- Training healthcare workers: Ensuring that healthcare workers are well-trained in handling pandemics and equipped with the necessary resources is crucial. There is also a need for mental health support for healthcare professionals, who are at the frontline during health crises.
- Leveraging technology: The use of telemedicine, mobile health applications, and digital platforms for remote consultations and monitoring of patients can help alleviate the burden on healthcare facilities during a pandemic.
2. Improved Early Warning and Surveillance Systems
A key challenge during the COVID-19 pandemic was the inability to detect and respond quickly to the spread of the virus. Effective early warning and surveillance systems are vital in detecting potential health threats early and preventing widespread outbreaks.
- Investing in data collection and analytics: Strengthening national surveillance systems and ensuring real-time data collection are essential for monitoring infectious diseases. This involves using advanced technology such as artificial intelligence (AI) and data analytics to predict and track outbreaks.
- Collaborating with international partners: Global collaboration and sharing of information are critical in detecting and managing pandemics. Kenya must continue to work with international health organizations like the World Health Organization (WHO) and neighboring countries to strengthen its surveillance networks.
3. Faster Response Mechanisms and Supply Chain Management
The pandemic highlighted the importance of having rapid response mechanisms in place. The global demand for medical supplies often outpaced supply, leaving countries like Kenya scrambling for essential equipment.
- Improving supply chain resilience: Investing in local production of medical supplies and diversifying supply chains can help ensure that Kenya is not overly reliant on imports during a health crisis. This includes increasing the capacity of local manufacturers to produce vaccines, medical equipment, and pharmaceuticals.
- Efficient distribution networks: Streamlining the distribution of essential supplies is crucial for ensuring that medical goods reach those in need without delay. Kenya must focus on building more efficient distribution systems, particularly in remote areas.
4. Public Health Education and Awareness
Public health education is vital in managing the spread of infectious diseases. The COVID-19 pandemic showed that misinformation, fear, and a lack of awareness could hinder efforts to control the virus.
- Combating misinformation: During the pandemic, there was a significant amount of misinformation circulating through social media. The government must work with media outlets and community leaders to provide accurate, reliable information to the public.
- Community engagement: Engaging local communities in health education and encouraging behavioral change through grassroots initiatives can ensure that public health messages reach everyone, particularly in rural and marginalized areas.
Steps Kenya is Taking to Prepare for Future Pandemics

1. Developing a National Pandemic Preparedness Plan
In the wake of COVID-19, Kenya has committed to developing a comprehensive national pandemic preparedness plan. This plan will focus on improving early warning systems, stockpiling essential medical supplies, and ensuring that healthcare systems can respond quickly to future outbreaks.
- Collaboration with regional bodies: Kenya is working closely with the East African Community (EAC) and other regional organizations to ensure that pandemic preparedness is coordinated across borders. This collaboration can help facilitate the sharing of resources and expertise during health emergencies.
- Public-private partnerships: The government is encouraging private sector involvement in pandemic preparedness, particularly in areas such as manufacturing medical supplies and providing logistical support.
2. Expanding Access to Health Insurance
Access to affordable healthcare is a major concern in Kenya, particularly during pandemics. Expanding the National Health Insurance Fund (NHIF) and making health insurance more accessible to low-income families can ensure that more people have access to the care they need during health emergencies.
- Universal health coverage (UHC): Kenya’s ongoing efforts to achieve universal health coverage will play a significant role in ensuring that every citizen has access to quality healthcare during a pandemic. This includes improving healthcare access in remote and underserved areas.
3. Fostering Regional and International Cooperation
Kenya is actively fostering regional and international cooperation to address the challenges posed by pandemics. By sharing data, resources, and expertise, Kenya and its neighbors can strengthen their collective response to health crises.
- African Union (AU) Health Strategy: Kenya is supporting the African Union’s efforts to improve the continent’s pandemic preparedness, including the establishment of an African Medicine Agency to ensure the availability of essential drugs and vaccines during health emergencies.
Conclusion
The COVID-19 pandemic revealed both the strengths and weaknesses of Kenya’s public health system. However, the lessons learned have spurred significant reforms and improvements that will enhance the country’s preparedness for future pandemics. By investing in healthcare infrastructure, strengthening surveillance systems, improving supply chains, and prioritizing public health education, Kenya is taking proactive steps to ensure that it is better prepared to handle the next health crisis.
The pandemic also highlighted the importance of regional and international cooperation, and Kenya is committed to collaborating with its neighbors and global health organizations to prevent and manage future pandemics effectively. As the country continues to build on the lessons learned from COVID-19, Kenya is laying the groundwork for a more resilient healthcare system that can withstand the challenges of the future.
This structured approach to pandemic preparedness will ensure that Kenya is not only ready for future health emergencies but also better equipped to manage their impact on public health and the economy.
References






